

No speciation was performed on the cultures. The results were reported quantitatively, and growth of 100,000 cfu/mL was considered positive. The container was then immediately taken to the microbiology laboratory, where the aspirate was cultured for aerobic bacteria. At endoscopy, duodenal aspirates were obtained via an aspiration catheter (Hobbs Medical Inc., Stafford Springs, CT, USA) and passed through the working channel of the upper endoscope (Olympus America Inc.) and its tip was positioned beyond the third or fourth part of the duodenum in order to avoid any potential contamination, no suction of any esophagogastricduodenal secretions was performed prior to the positioning of the aspiration catheter in the duodenum The small bowel fluid was suctioned into a sterile container and at least 1 mL was obtained. Indications for the procedure, demographic information, and endoscopic findings were recorded from the endoscopy reports. A list of these patients was retrieved from our endoscopy database. The study was a retrospective review of patients undergoing outpatient EGD with duodenal aspirates at Mayo Clinic Arizona between January and December 2012. We hypothesized that PPI use would be associated with higher rates of positive duodenal aspirate culture in our population. We sought to evaluate a cohort of patients undergoing EGD with duodenal aspirates to determine the diagnostic yield of cultures, clinical response to antibiotic treatment and the risk factors associated with SIBO.Īlthough there is controversy regarding the association between PPI therapy and SIBO, a recent meta-analysis has suggested a positive association only when the diagnosis of SIBO is based on aspiration cultures. SIBO has been associated with conditions affecting GI motility, such as gastroparesis and scleroderma, gastrointestinal surgery, small bowel diverticula, immunologic disorders, such as IgA deficiency and combined variable immunoglobulin deficiency, and conditions associated with decreased gastric acid secretion. Although breath tests have not been standardized, they may also serve as indirect evidence of SIBO when they are positive. The diagnosis requires a positive culture defined as >100,000 colony forming units per mL (cfu/mL) in aspirates obtained from the small bowel however, some have used the less frequent and not as reliable cutoff of 10,000 cfu/mL. Small intestinal bacterial overgrowth (SIBO) is a clinical entity that may be responsible for a constellation of symptoms that include bloating, abdominal distension, pain, and diarrhea.

Similar proportions of patients with SIBO improved whether or not they received antibiotic treatment, calling into question the use of this expensive therapy for this disorder. A significantly higher percentage of patients with SIBO use PPIs than patients without SIBO, indicating a possible association. Culture analysis of duodenal aspirates identified SIBO in one-third of patients. Aspirates were collected thought out the third and fourth portions of the duodenum, and cultures were considered to be positive for SIBO if they produced more than 100,000 cfu/mL. In a retrospective study, we analyzed electronic medical records from 1263 consecutive patients undergoing upper endoscopy at a tertiary medical center. We aimed to determine the yield of SIBO-positive cultures detected in duodenal aspirates, the relationship between SIBO and PPI use, and the clinical outcomes of patients identified by this method. Proton pump inhibitor (PPI) use has been proposed to contribute to the development of SIBO.
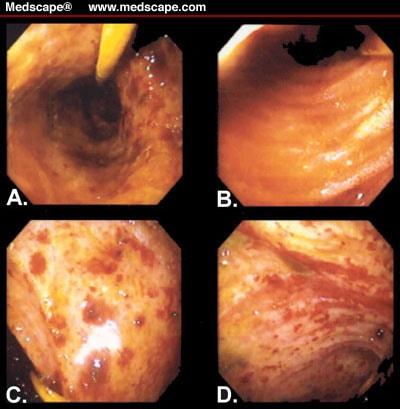
Duodenal aspirates are not commonly collected, but they can be easily used in detection of small intestinal bacterial overgrowth (SIBO).


 0 kommentar(er)
0 kommentar(er)
